Procedures
Gastroenterology Procedures
Colonoscopy
What is a Colonoscopy?
Colonoscopy is a procedure that enables your physician to examine the lining of the colon (large bowel) for abnormalities by inserting a flexible tube that is about the thickness of your finger into the anus and advancing it slowly into the rectum and colon.
What preparation is required?
The colon must be completely clean for the procedure to be accurate and complete. Your physician will give you detailed instructions regarding the dietary restrictions to be followed and the cleansing routine to be used. In general, preparation consists of either consumption of a large volume of a special cleansing solution or several days of clear liquids, laxatives, and enemas prior to the examination. Follow your doctor’s instructions carefully. If you do not, the procedure may have to be canceled and repeated later.What about my current medications?
Most medications may be continued as usual, but some medications can interfere with the preparation or the examination. It is therefore best to inform your physician of your current medications as well as any allergies to medications several days prior to the examination. Aspirin products, arthritis medications, anticoagulants (blood thinners), insulin, and iron products are examples of medications whose use should be discussed with your physician prior to the examination.What can be expected during colonoscopy?
Colonoscopy is usually well tolerated and rarely causes much pain. There is often a feeling of pressure, bloating, or cramping at times during the procedure. Your doctor may give you medication through a vein to help you relax and better tolerate any discomfort from the procedure. You will be lying on your side or on your back while the colonoscope is advanced slowly through the large intestine. As the colonoscope is slowly withdrawn, the lining is again carefully examined. The procedure usually takes 15 to 60 minutes. In some cases, passage of the colonoscope through the entire colon to its junction with the small intestine cannot be achieved. The physician will decide if the limited examination is sufficient or if other examinations are necessary.What if the colonoscopy shows something abnormal?
If your doctor thinks an area of the bowel needs to be evaluated in greater detail, a forceps instrument is passed through the colonoscope to obtain a biopsy (a sample of the colon lining). This specimen is submitted to the pathology laboratory for analysis. If colonoscopy is being performed to identify sites of bleeding, the areas of bleeding may be controlled through the colonoscope by injecting certain medications or by coagulation (sealing off bleeding vessels with heat treatment). If polyps are found, they are generally removed. None of these additional procedures typically produce pain. Remember, the biopsies are taken for many reasons and do not necessarily mean that cancer is suspected.What are polyps and why are they removed?
Polyps are abnormal growths from the lining of the colon which vary in size from a tiny dot to several inches. The majority of polyps are benign (noncancerous) but the doctor cannot always tell a benign from a malignant (cancerous) polyp by its outer appearance alone. For this reason, removed polyps are sent for tissue analysis. Removal of colon polyps is an important means of preventing colorectal cancer.How are polyps removed?
Tiny polyps may be totally destroyed by fulguration (burning), but larger polyps are removed by a technique called snare polypectomy. The doctor passes a wire loop (snare) through the colonoscope and severs the attachment of the polyp from the intestinal wall by means of an electrical current. You should feel no pain during the polypectomy. There is a small risk that removing a polyp will cause bleeding or result in a burn to the wall of the colon, which could require emergency surgery.What happens after a colonoscopy?
After colonoscopy, your physician will explain the results to you. If you have been given medications during the procedure, someone must accompany you home from the procedure because of the sedation used during the examination. Even if you feel alert after the procedure, your judgment and reflexes may be impaired by the sedation for the rest of the day, making it unsafe for you to drive or operate any machinery.You may have some cramping or bloating because of the air introduced into the colon during the examination. This should disappear quickly with passage of flatus (gas). Generally, you should be able to eat after leaving the endoscopy, but your doctor may restrict your diet and activities, especially after polypectomy.
What are the possible complications of colonoscopy?
Colonoscopy and polypectomy are generally safe when performed by physicians who have been specially trained and are experienced in these endoscopic procedures. One possible complication is a perforation or tear through the bowel wall that could require surgery. Bleeding may occur from the site of biopsy or polypectomy. It is usually minor and stops on its own or can be controlled through the colonoscope. Rarely, blood transfusions or surgery may be required. Other potential risks include a reaction to the sedatives used and complications from heart or lung disease. Localized irritation of the vein where medications were injected may rarely cause a tender lump lasting for several weeks, but this will go away eventually. Applying hot packs or hot moist towels may help relieve discomfort. Although complications after colonoscopy are uncommon, it is important for you to recognize early signs of any possible complication. Contact vour physician who performed the colonoscopy if you notice any of the following symptoms: severe abdominal pain. fever and chills, or rectal bleeding of more than one- half cup. Bleeding can occur several days after polypectomy.Flexible
Sigmoidoscopy
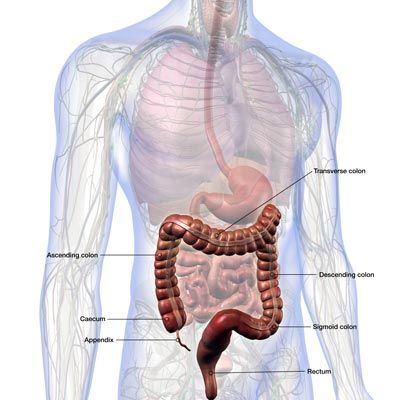
Flexible sigmoidoscopy enables the physician to look at the inside of the large intestine from the rectum through the last part of the colon, called the sigmoid or descending colon with the use of an endoscope. This examination is typically used to evaluate complaints of rectal bleeding, constipation, diarrhea and pain in the left lower quadrant or pelvis.
It is important for your doctor to have a clear view of your colon during the examination, you will be given instructions from your physician as to the preparation to use prior to the examination.
Flexible sigmoidoscopy enables the physician to look at the inside of the large intestine from the rectum through the last part of the colon, called the sigmoid or descending colon with the use of an endoscope. This examination is typically used to evaluate complaints of rectal bleeding, constipation, diarrhea and pain in the left lower quadrant or pelvis.
It is important for your doctor to have a clear view of your colon during the examination, you will be given instructions from your physician as to the preparation to use prior to the examination.
The examination is a quick procedure with minimal complications. Usually, patients are not sedated for this procedure. During the procedure you may experience the sensations you feel prior to a bowel movement. You will be asked to lie on your left side on the examining table. The physician will insert a short, flexible, lighted tube into your rectum and slowly guide it into your colon. The tube is called a sigmoidoscope. The scope has a camera on the distal tip which enables the physician to carefully examine the lining of your colon. If anything unusual is in your rectum or sigmoid colon, such as a polyp or inflamed tissue, the physician can remove a sample using an instrument inserted into the scope. The tissue can then be sent to the lab for evaluation.
The examination is a quick procedure with minimal complications. Usually, patients are not sedated for this procedure. During the procedure you may experience the sensations you feel prior to a bowel movement. You will be asked to lie on your left side on the examining table. The physician will insert a short, flexible, lighted tube into your rectum and slowly guide it into your colon. The tube is called a sigmoidoscope. The scope has a camera on the distal tip which enables the physician to carefully examine the lining of your colon. If anything unusual is in your rectum or sigmoid colon, such as a polyp or inflamed tissue, the physician can remove a sample using an instrument inserted into the scope. The tissue can then be sent to the lab for evaluation.
Flexible sigmoidoscopy takes 10 to 20 minutes. Flexible sigmoidoscopy is usually well tolerated and rarely causes much pain. There is often a feeling of pressure, bloating, or cramping at various times during the procedure and for a short period after the procedure.
Bleeding and puncture of the colon are possible complications of flexible sigmoidoscopy. However, such complications are uncommon.
Most medications can be continued as usual. You should inform your physician if you are taking blood thinners or if you require antibiotics prior to undergoing dental procedures.
ERCP
What is ERCP?
ERCP is a specialized technique used to study the ducts (drainage routes) of the gallbladder, pancreas, and liver (the drainage channels from the liver are called bile ducts or biliary ducts). An endoscope (flexible thin tube that allows the physician to see inside the bowel) is passed through the mouth, esophagus, and stomach into the duodenum (first part of the small intestine). After the common opening to ducts from the liver and pancreas is visually identified, a catheter (narrow plastic tube) is passed through the endoscope into the ducts. Contrast material (“dye”) is then injected gently into the ducts (pancreatic or biliary) and x-ray films are taken.

What preparation is required?
It is necessary to have a completely empty stomach for the best possible examination. You should therefore fast for at least 6 hours (and preferably overnight) before the procedure. An allergy to iodine containing drugs (contrast material or “dye”) is not a contraindication to ERCP, but it should be discussed with your physician prior to the procedure. The physician performing the procedure should be informed of any medications that you take regularly, any heart or lung conditions (or any other major diseases), and whether you have any drug allergies.
Someone must accompany you home from the procedure because of the sedation used during the examination. Even if you feel alert after the procedure, your judgment and reflexes may be impaired by the sedation for the rest of the day, making it unsafe for you to drive or operate any machinery. If a complication occurs, you may need to be hospitalized until it resolves.
What can be expected during ERCP?
Your physician will discuss why ERCP is being performed, potential complications from ERCP, and alternative diagnostic or therapeutic tests that are available. A local anesthetic may be applied to your throat and an intravenous sedative may be given to make you more comfortable during the test. Some patients also receive antibiotics before the procedure. The test begins with you lying on your left side on an x-ray table. The endoscope is passed through the mouth, esophagus, and stomach into the duodenum. The instrument does not interfere with breathing. Air is introduced through the instrument and may cause temporary bloating during and after the procedure. The injection of contrast material into the ducts rarely causes discomfort.
What are possible complications of ERCP?
ERCP is generally a well-tolerated procedure when performed by physicians who have had special training and experience in this technique. Localized irritation of the vein into which medications were given may rarely cause a tender lump that may last several weeks. The application of heat packs or hot moist towels to the area may ease the discomfort.
Major complications requiring hospitalization can occur but are uncommon during diagnostic ERCP. They include serious pancreatitis and even more rarely infections, bowel perforation, and bleeding. Another potential risk of ERCP is an adverse reaction to the sedative used. The risks of the procedure vary with the indications for the test, what is found during the procedure, what therapeutic intervention is undertaken, and the presence of other major medical problems, eg, heart or lung diseases. Your physician will tell you what is your likelihood of complications before undergoing the test.
If therapeutic ERCP is performed (cutting an opening in the bile duct, stone removal, dilation of a stricture, stent or drain replacement, etc), the possibility of complications is higher than with diagnostic ERCP; complications include pancreatitis, bleeding, and bowel perforation. These risks must be balanced against the potential benefits of the procedure and the risks of alternative surgical treatment of the condition. Often these complications can be managed without surgery, but occasionally they do require corrective surgery.
What can be expected following ERCP?
If you are having ERCP as an outpatient, you will be kept under observation until most of the effects of the medications have worn off. Evidence of any complications of the procedure will be looked for and hospitalization may be advised if further observation is necessary. You may experience bloating or pass gas because of the air introduced during the examination. You may resume your usual diet unless you are instructed otherwise.
To the patient Because education is an important part of comprehensive medical care, you have been provided with this information to prepare you for this procedure. If you have any questions about your need for ERCP, alternative approaches to your problem, the cost of the procedure.
Capsule Endoscopy
Small Bowel Capsule Endoscopy
Capsule endoscopy assists in diagnosing gastrointestinal conditions such as bleeding, malabsorption, abdominal pain, tumors, Crohn’s Disease, infectious enteritis, celiac sprue and drug-induced ulceration. Capsule endoscopy can help your physician determine the cause for recurrent or persistent symptoms such as diarrhea, bleeding or anemia. The physician can also use capsule endoscopy to obtain motility data such as gastric or small bowel passage time, help to evaluate the extent to which your small intestine is involved, or monitor the effect of therapy.
The capsule endoscope, utilizes a wireless video camera, small enough to swallow, to perform painless endoscopic imaging of the small intestine. Thousands of video images of the gastrointestinal tract are transmitted by sensors attached to the patient’s abdomen. These images are stored on a data recorder worn by the patient and later downloaded onto a computer for viewing by the physician.
Upper GI Endoscopy
Upper endoscopy is a procedure performed to enable your physician to examine the lining of the upper part of your gastrointestinal tract. The upper part of your gastrointestinal tract includes your esophagus, stomach, and duodenum. The upper endoscopy is performed to diagnose and, in some cases, treat problems of the upper digestive system. The procedure is performed using a flexible endoscope.The flexible endoscope is a long, thin, flexible tube with a tiny camera and light on the end. The endoscope projects high quality pictures on a monitor which enables the physician to carefully examine the inside lining of the upper digestive system.
Why is upper endoscopy done?
The upper endoscopy is performed to evaluate symptoms of persistent upper abdominal pain, nausea, vomiting, or difficulty swallowing. It is also the best test for finding the cause of bleeding from the upper gastrointestinal tract.
What preparation is required?
You should have nothing to eat or drink, including water, after midnight the day before your procedure. Your physician will be more specific about the time to begin fasting, depending on the time of day your test is scheduled.
You will need to inform your physician of your current medications as well as any allergies several days prior to the procedure. You need to inform your physician if you have a pacemaker or defibrillator or any major disease that might require special attention during the procedure.
Arrangements to get home after the test
If you are sedated, you will need to arrange to have someone to drive you home after the examination. The sedatives may affect your judgment and reflexes the rest of the day, you should not drive, operate any machinery, or make any important decisions.
What can be expected during the upper endoscopy?
Your physician will review with you why this test is being performed, whether any alternative tests are available and possible complications from the procedure. You will have medication given through an IV to sedate you, a latex free mouthpiece will be placed between your teeth to protect your teeth and the instrument. The endoscope will be passed through the mouthpiece, then the esophagus, stomach and duodenum. The endoscope does not interfere with your breathing during the test. Your blood pressure, heart rhythm, and oxygen saturation will be carefully monitored throughout the procedure.
What happens after endoscopy?
After the test you will be monitored in the recovery area until most of the effects of the medication have worn off. You will be given instructions regarding how soon you can eat and drink, and guidelines for resuming normal activities.
Occasionally, minor problems may persist, such as a mild sore throat, bloating, or cramping; these should disappear within 24 hours or less.
In most cases, your physician can inform you of your test results on the day of the procedure; however, the results of any biopsies or cytology samples taken will take two to three days.
What are the possible complications of upper endoscopy?
Endoscopy is generally safe. Complications can occur but are rare. Bleeding may occur from a biopsy site or where a polyp was removed. Localized irritation of the vein where the medication was injected may rarely cause a tender lump lasting for several weeks. Applying heat packs or hot moist towels may help relieve the discomfort. Other potential risks include a reaction to the sedatives used and complications from heart or lung diseases. Perforation (a tear that might require surgery) could possible occur but is very uncommon.
It is important to recognize early signs of any possible complications. If you begin to run a temperature after your procedure, begin to have trouble swallowing, or have increasing throat, chest, or abdominal pain, let you physician know immediately.
Endoscopic Ultrasound
What is an Endoscopic Ultrasound (EUS)?
For many patients who have, or who are suspected of having pancreatic disease, their doctor may recommend that they undergo a type of procedure called an endoscopic ultrasound, or more often known as EUS.
An EUS is a type of endoscopic examination. It involves the insertion of a thin tube into the mouth and down into the stomach and the first part of the small intestine. At the tip of the tube is a small ultrasound probe that emits sound waves. These sound waves bounce off of the surrounding structures, such as the stomach, small intestine, pancreas, bile ducts, and liver. These sound waves are then recaptured by the probe and converted into black and white images that are then interpreted by your doctor. Because the pancreas sits next to the stomach and small intestine, EUS allows the physician to get very detailed images of the pancreas. This procedure is typically performed in an outpatient setting, and usually takes between 20 and 45 minutes.
What are the reasons why I need an EUS?
EUS allows for very detailed imaging and analysis of the pancreas. As such, it is an excellent test for evaluating many different kinds of diseases that can occur in the pancreas. Examples of such pancreatic conditions for which EUS can be extremely useful are:
- Pancreatic masses and tumors
- Pancreatic cysts
- Chronic pancreatitis
- Autoimmune pancreatitis
- Acute pancreatitis
One of the most common reasons that patients are referred for an EUS of the pancreas is to evaluate abnormal findings on a CT (CAT scan), MRI, or ultrasound of the abdomen, or for further investigation of abnormal blood tests such as elevated liver function tests (AST, ALT, bilirubin) or elevated pancreatic enzymes (amylase, lipase). Patients with certain types of abdominal pain may also be referred for an EUS. Examples of reasons for referral for an EUS include:
- Dilated pancreatic duct
- Dilated bile duct
- Swollen/inflamed pancreas
- Suspected stones in the pancreas duct or bile duct
- Suspected blockage of the pancreas or bile duct
- History of recurrent episodes of acute pancreatitis
These findings listed above can be caused by both benign and malignant conditions. Thus, it is important that you discuss the reason for the EUS with your physician.
Can biopsies of the pancreas be taken at the time of my EUS?
One of the advantages of performing an EUS is that pancreatic biopsies can be obtained at the time of the examination. These biopsies, often referred to as FNA, or fine-needle aspiration, can allow for your physician to collect tissue samples which can later be analyzed under a microscope. Special needles, designed to be used with the EUS scope, allow the physician to insert a small needle through the wall of the stomach or intestine directly into the pancreas. Because this is done at the time of the EUS, the physician is able to direct the needle to the exact location of interest all while watching the needle with the EUS.
FNA is most commonly performed to evaluate masses or tumors of the pancreas, in order to determine if cancer is present. Another very common reason for performing an FNA is in the evaluation of pancreatic cysts. In these cases, the needle is used to sample the fluid which is contained in the cyst. This fluid can be sent for biochemical, cytologic, and molecular analysis in order to help characterize the type of pancreatic cyst you have.
In certain circumstances, larger biopsy samples of the pancreas may be required. EUS allows the physician to obtain “core biopsies” of the pancreas in a similar fashion to FNA.
What are the advantages of an EUS, compared to a CT scan, MRI, or ERCP?
There are many different tests which can be used to evaluate the pancreas. CT scans and MRI are types on non-invasive tests which allow for detailed imaging of the pancreas and the surrounding structures in the abdominal cavity. CT scans expose the patient to some amount of radiation. Furthermore, some patients are unable to receive IV contrast for their CT scans (due to allergies or kidney problems), and thus the quality of the pictures will be sub-optimal. A special kind of MRI called an MRCP can give high-quality pictures of the pancreas, the pancreas duct, and the bile ducts. However, some patients who are claustrophobic may decide against having an MRI performed.
As discussed, EUS allows the physician to get in very close proximity to the pancreas, which results in very detailed imaging of the organ. The endoscopist can often times visualize details of the pancreas that cannot be seen with either CT or MRCP. Furthermore, there is no exposure to radiation and no need for contrast to be given. In addition, because the EUS scope has a video camera on it, endoscopic evaluation of the esophagus, stomach, and first part of the small intestine can also be evaluated at the time of the EUS. This is important for some patients who are having a work-up for abdominal pain as it allows for a complete examination of the upper GI system.
The biggest advantage of EUS is that, unlike with CT or MRCP, pancreatic biopsies can be safely and easily obtained at the time of the exam.
Are there any risks of having an EUS?
Because sedation, or in some cases, general anesthesia is used during EUS, there is a risk for cardiac and/or pulmonary complications during an EUS procedure.
As with any endoscopic procedure, there is a small risk of causing bleeding or a tear of the GI tract (called a perforation). These complications can often be managed endoscopically, however emergency surgery may be required in the worst case scenario. Fortunately, the risk of a severe complication like this from EUS is very low, less than 1% of the time in most cases.
Biopsies/FNA of the pancreas can also result in bleeding, infection, or acute inflammation of the pancreas (called acute pancreatitis). FNA of pancreatic cysts can result in infection of the cyst. This has been reported to occur in 1-2% of cases. Your physician may give you an antibiotic during the procedure to prevent infection, and may prescribe a short course of oral antibiotics after the procedure.
How should I prepare for my EUS?
You should not have anything to eat or drink for approximately 8 hours before your EUS. Typically, patients are asked to refrain from eating or drinking after midnight the night before their test.
Your physician may ask you to hold any blood thinning medications for one week before your test. Examples include aspirin, Plavix, and coumadin. You may be allowed to take your other medications on the morning of your test. It is extremely important that you tell your physician what medications you are on, and discuss if any need to be stopped before the test.
If you have a history of heart or lung disease, you may be required to get a letter from your heart or lung doctors stating that it is safe for you to have an endoscopy and receive sedation.
What should I expect on the day of my EUS?
On the day of your EUS, you will arrive in the endoscopy suite. An IV catheter will be placed in your hand or arm so that you can receive intravenous fluids and sedatives during the procedure.
Once you are brought into the endoscopy room, you will lay down on a bed, usually on your left side (like you are watching TV). In order to monitor your vital signs during the procedure, a blood pressure cuff will be placed on your arm, an oxygen monitor will be placed on your finger, and EKG leads will be placed on your chest. A small nasal cannula will be placed in your nose to give you oxygen during the procedure. A small plastic “bite block” will be placed in your mouth between your teeth, which protects your teeth and prevents any accidental biting of the scope during the procedure.
Sedatives will be injected into your IV before the procedure begins. The procedure usually lasts from 20-45 minutes, but can be shorter or longer. The vast majority of patients do not feel or experience any discomfort during the procedure, as they are usually asleep during the procedure.
When the procedure is finished, you will be brought to a recovery area where you will lay in bed until you are awake. Your vital signs will continue to be monitored during this time. When you are awake, you will be given some juice and a small snack. The recovery period usually lasts between 20 minutes to 1 hour.
Before you are discharged home, you will have an opportunity to meet with your physician to discuss the results of the EUS, and receive further instructions regarding your medications.
Infusion Therapy
The infusion center has both a large infusion area and private treatment rooms. Our nursing staff provides compassionate personalized care during your infusion in a relaxed and comfortable setting.
Office IV Infusion Therapy
Usually, a medically stable patient does not need to be admitted to the hospital for certain therapy. As a result, the patient can receive treatment in the office infusion center. This involves the administration of the prescribed medication(s) intravenously or with some drugs via injection. The DDC infusion center currently provides Remicade and Entyvio I.V. therapy.
Biologic Medications For Immune Mediated Inflammatory Disease (IMID)
Biologic therapy is indicated for reducing the signs and symptoms including maintaining clinical remission in patient's with moderate to severe diseases such as Crohn's Disease, Ulcerative Colitis. A PPD, Chest X-ray, and lab work must be obtained within one year of referral date and prior to administrations of all biologic medications. These patients may be considered for biologic therapy that are classified as IMID and have not responded to conventional therapy or are not candidates for other medications.
Remicade
Remicade is FDA approved for all IMID diagnoses. It is based on patient weight so each dose is made uniquely for that patient at the time of their infusion appointment. It is infused every 8 weeks over two hours at the minimum, but can be infused over a longer time interval based on the needs of the individual.

Entyvio
Developed for ulcerative colitis and Crohn's, ENTYVIO works by focusing right in the GI tract to help control damaging inflammation. Individual results may vary.

Crohn’s Disease
Ulcerative Colitis
Hemorrhoid Banding
Flexible sigmoidoscopy enables the physician to look at the inside of the large intestine from the rectum through the last part of the colon, called the sigmoid or descending colon with the use of an endoscope. This examination is typically used to evaluate complaints of rectal bleeding, constipation, diarrhea and pain in the left lower quadrant or pelvis.
It is important for your doctor to have a clear view of your colon during the examination, you will be given instructions from your physician as to the preparation to use prior to the examination.
The CRH O'Regan System treats hemorrhoids completely - without surgery or recovery time.
The hemorrhoid treatment process is simple. The procedure is easy, fast and painless. You’ll be amazed at how simple it is…and how great you feel. Just find a physician to make an appointment to see if CRH is right for you.
The CRH O’Regan hemorrhoid treatment technology works by cutting off the blood supply to the hemorrhoid, causing it to shrink and fall off in a few days. You may not even notice when this happens.
Fewer than 5% of patients have a recurrence within 2 years
Takes less than 1 minute
Less than 1% complication rate — much safer than traditional banding
With our unique banding system, you won’t feel pain or need to take valuable time off work. Hemorrhoid treatment with the CRH system is even covered by most insurance plans. See why the CRH O’Regan System is considered more than 99% effective in treating hemorrhoids. Learn more about our treatment here: https://www.crhsystem.com/crh-oregan-system
What to Know Before Your Hemorrhoid Banding Appointment?
Every physician in the CRH network works hard to ensure your hemorrhoids are treated completely; after hemorrhoid banding, you’ll be without pain or downtime. Before your appointment, you don’t even need to fast or take other measures to prepare.
Here's what to expect on your first visit:
During your Hemorrhoid Banding Appointment
First, your physician will examine you and confirm your diagnosis. If he or she determines a CRH System hemorrhoid banding procedure is right for you, you may begin treatment right away, or on a subsequent visit.
During the brief and painless banding procedure, your physician will use a gentle suction device – unlike the harsh metal clamps used in other banding treatments – to place a small rubber band around the base of the internal hemorrhoid where there are no pain-sensitive nerve endings. The whole thing typically takes less than 60 seconds.
After the Hemorrhoid Banding Appointment
Once the band is in place, it cuts off the blood supply to the hemorrhoid, causing the banded tissue to fall off, typically within a few days. You probably will not even notice when this happens! The hemorrhoid will shrink, relieving your symptoms.
During the first 24 hours, you may experience a feeling of fullness or a dull ache in the rectum, but over-the-counter pain medication will provide sufficient relief.
If you have multiple hemorrhoids, you’ll likely need to come back to treat each one separately – that way, your doctor can monitor your treatment and ensure the complication rate is kept to an absolute minimum.
After your Hemorrhoid Banding Appointment, recovery is easy.
The examination is a quick procedure with minimal complications. Usually, patients are not sedated for this procedure. During the procedure you may experience the sensations you feel prior to a bowel movement. You will be asked to lie on your left side on the examining table. The physician will insert a short, flexible, lighted tube into your rectum and slowly guide it into your colon. The tube is called a sigmoidoscope. The scope has a camera on the distal tip which enables the physician to carefully examine the lining of your colon. If anything unusual is in your rectum or sigmoid colon, such as a polyp or inflamed tissue, the physician can remove a sample using an instrument inserted into the scope. The tissue can then be sent to the lab for evaluation.
Browse Our Website
Contact Information
Phone: (850) 877-2105
Email: [email protected]
Fax:
(850) 942-1761
Address: 2400 Miccosukee Road, Tallahassee, FL 32308
Hours of Operation
- Mon - Thu
- -
- Friday
- -
- Sat - Sun
- Closed
Visit Our Location
Digestive Disease Clinic © 2018 | Powered by: SoftAge Systems, Inc. | Privacy Policy
| Notice of Nondiscrimination
Content, including images, displayed on this website is protected by copyright laws. Downloading, republication, retransmission or reproduction of content on this website is strictly prohibited. Terms of Use
| Privacy Policy